Balance disorders in the elderly
Balance disorders are a common condition in the elderly, but often still poorly managed. With technological and medical advances in recent years, these problems are no longer inevitable.
Common among the elderly, balance disorders are often connected to the inability to properly use and centrally integrate the sensory information necessary for balance.
Leucoaraiose vasculaire
“Your problems are related to your age, you’re not twenty any more, you’ll have to get used to it”. This is what the elderly suffering from balance disorders generally hear, and the traditional physiotherapy sessions offered often do nothing to help. Balance disorders, however, are common in the elderly, and have many, sometimes serious, repercussions on their everyday life: the feeling of inebriation, pitching, unsteadiness, fear of going down stairs, etc. But also the risk of falls, which of course can be very dangerous. To give just one example, falls are the second leading cause of death among the elderly, after cardiovascular events. It is therefore important not to take these disorders lightly, especially as there are now new appropriate treatments.
Otoneurological assessment
With a patient suffering from balance problems, the first step should be a functional otoneurological assessment of the inner ear to detect any possible disease of the latter. This assessment includes the audiometric and vestibular tests described above.

Exploring balance disorders
The physician searches for balance disorders using various tools to help understand their causes when the inner ear functional test is normal. Examining patients’ balance on a fixed platform enables an initial assessment of their static posturography eyes open and closed. Often, this test provides little guidance for the otoneurologist, as proprioception and vestibular inputs, even though they may be deficient in everyday life, are sufficient to maintain a normal balance while standing on a static platform. Examining the dynamic posturography on a moving platform gives a greater variety of information.
Placing patients on a foam mat 8 cm in height with their eyes closed will, for example, give the clinician information on any anomaly in balance, which can be quantified if the foam mat is positioned on a static computerised platform.
Dynamic posturography on a moving platform also provides important information about patients with a unilateral or bilateral vestibular condition. With their eyes closed and if suffering from unilateral areflexia, patients fail to maintain their balance when the platform moves side to side but are able to do so with a forwards-backwards motion. With bilateral vestibular areflexia, patients fall when their eyes are closed, whether the motion is side to side or forwards-backwards.
The EquiTest or multisensory test
The EquiTest is the reference tool to assess how well patients use the various types of sensory information to maintain their balance. It enables the physician to quantify balance disorders and to assess whether the vestibular, visual or proprioceptive input is used correctly. It is also useful for rehabilitation: it enables patients to correct their poor use of the visual, vestibular or proprioceptive sensory information in everyday life. The ultimate goal of this rehabilitation method is to prevent falls and their often harmful functional consequences.
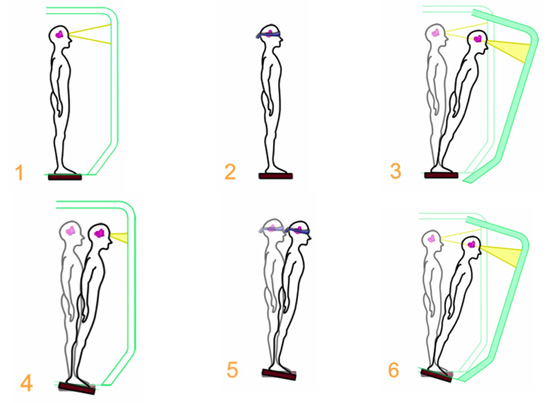
The EquiTest evaluates the sensory preference used to maintain balance
The EquiTest is used to measure the displacement of the vertical forces exerted by the patient’s feet under six conditions (see diagram below):
• maintaining balance with eyes open - C1);
• maintaining balance with eyes closed - C2);
• maintaining balance with eyes open with controlled vision (displacement of visual surround according to changes in the patient’s centre of gravity - C3);
• maintaining balance with eyes open with controlled proprioception (the platform moves in the sagittal plane according to the changes in the patient’s centre of gravity - C4);
• maintaining balance with eyes closed with controlled proprioception - C5); maintaining balance with eyes open with controlled proprioception and vision - C6).
A final score is given for each condition in three consecutive tests. It allows the physician to ascertain the sensory preference used by the patient to maintain balance. Patients making little or poor use of their vestibular information will, for example, show a poor performance or fall under conditions C5 and C6.
Equitest video
